How to Access the port?
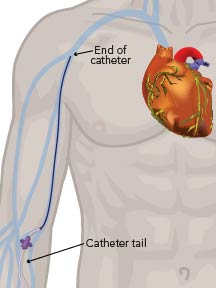
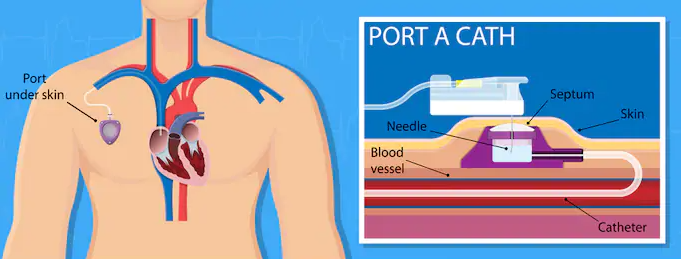
A port-a-cath also referred to as a port, is an implanted device that allows easy access to a patient’s veins. A port-a-cath is surgically-inserted completely beneath the skin and consists of two parts – the portal and the catheter.
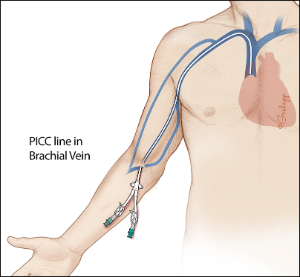
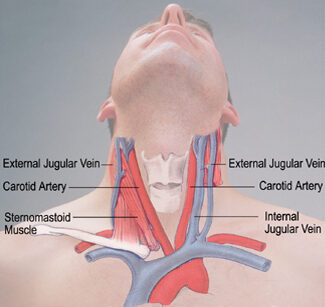
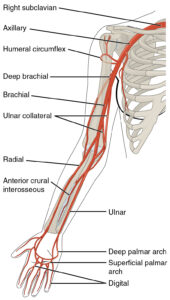
The portal is typically made from a silicone bubble and appears as a small bump under the skin. The portal, made of special self-sealing silicone, can be punctured by a needle repeatedly before the strength of the material is compromised. Its design contributes to a very low risk of infection. The slender, plastic catheter attached to the portal is threaded into a central vein (usually the jugular vein or subclavian vein and terminates in the superior vena cava).
What is the indication for a port-a-cath?
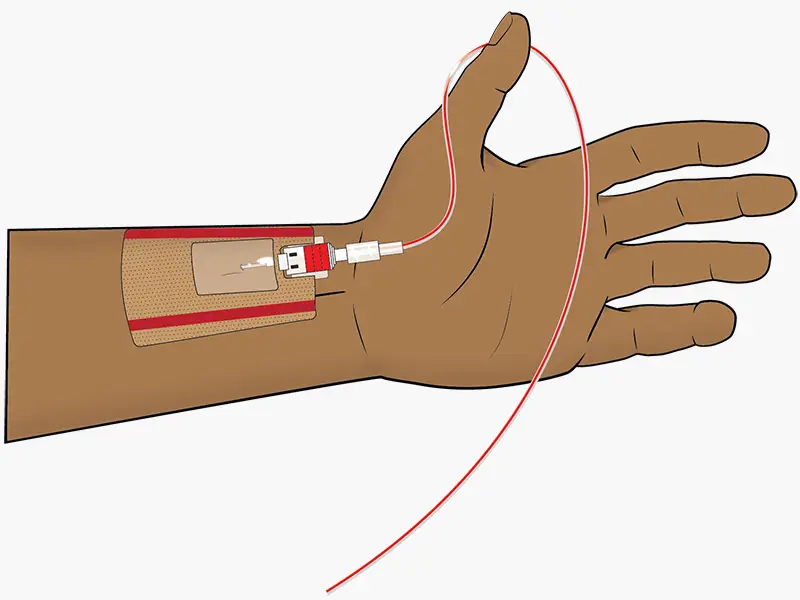
Ports are indicated for patients requiring frequent and long-term intravenous therapy, such as the oncology population. Having a port allows healthcare professionals easy access to a major vein with a low risk of infection.
This benefit is extremely important for the immunocompromised population of oncology patients. Additionally, it reduces the pain that would otherwise be experienced with countless needle pokes for IVs since the skin over a port hub becomes thicker and desensitized.
Another consideration is that oncology patients may receive chemotherapy often, which can be toxic and erosive to tissues in the body. By infusing chemotherapy through a strong vein via the port, the medication has a lower chance of leaking into tissues and causing extravasation or irritation.
Once a port is cleared for use, a patient may receive intravenous therapy through it for the course of his/her treatment. An adult portal chamber can take about 2,000 punctures on average, which may last a patient several years.